Η επιδημία της Πολυφαρμακίας-Polypharmacy
Ο όρος «πολυφαρμακία» συχνά χρησιμοποιείται στην ιατρική ορολογία για να περιγράψει τη «χρήση τουλάχιστο ενός δυνητικά ακατάλληλου για την πάθηση για την οποία χορηγείται φαρμάκου ή για να προσδιορίσει την ταυτόχρονη λήψη 5 και άνω φαρμακευτικών σκευασμάτων (Brager & Sloand, 2005).
Το φαινόμενο της πολυφαρμακίας είναι ιδιαίτερα έντονο σε ορισμένες ομάδες φαρμάκων, όπως Φάρμακα Καρδιαγγειακού, Υπνωτικά, Ψυχότροπα, Φάρμακα Αναπνευστικού, τα Αντιβιοτικά-που χρησιμοποιούνται άσκοπα σε ιογενείς λοιμώξεις-και τα ΜΣΑΦ (Μη Στεροειδή Αντιφλεγμονώδη Φάρμακα), που χρησιμοποιούνται κατά κόρον ως αναλγητικά, αντιπυρετικά καθώς και σε διάφορες μυοσκελετικές παθήσεις. Ιδιαίτερα στα ΜΣΑΦ το πρόβλημα γίνεται ακόμα εντονότερο, λόγω της κυκλοφορίας πολλών σκευασμάτων διαφορετικών εταιριών, αλλά της ίδιας δραστικής ουσίας, με αποτέλεσμα ο ασθενής να λαμβάνει δύο με τρία ίδια φάρμακα για τη θεραπεία μιας νόσου.
Η επιδημία της πολυφαρμακίας πλήττει κυρίως ανθρώπους της τρίτης ηλικίας, καθώς οι ηλικιωμένοι αποτελούν το 13% του συνολικού πληθυσμού και καταναλώνουν 30% και πλέον των συνταγογραφούμενων φαρμάκων. Πιο αναλυτικά, ο μέσος ασθενής ηλικίας άνω των 70 ετών παίρνει 4,5 φάρμακα με συνταγή και 5 χωρίς συνταγή, ενώ το 80% των ατόμων άνω των 65 ετών παίρνουν ένα φάρμακο την ημέρα.
Άλλες κατηγορίες ασθενών που κινδυνεύουν από το φαινόμενο της πολυφαρμακίας είναι οι ψυχιατρικοί ασθενείς, με συνυπάρχουσες παθήσεις καθώς και ασθενείς με προβλήματα όρασης και πνευματικής λειτουργίας.
Η πολυφαρμακία συναντάται συχνά στους χρήστες αναβολικών στεροειδών. Διάφορα φάρμακα λαμβάνονται με σκοπό είτε τη βελτίωση της αθλητικής απόδοσης είτε την αντιμετώπιση των ανεπιθύμητων δράσεων της χρήσης αναβολικών στεροειδών (Korkia P, Stimson, 1997). Η πολυφαρμακία οδηγεί:
Στην εμφάνιση ανεπιθύμητων ενεργειών με επίπτωση στην κατάσταση υγείας των ασθενών με συνεπακόλουθο την αυξημένη νοσηρότητα και θνητότητα. Όσο αυξάνεται ο αριθμός των φαρμάκων αυξάνεται και ο κίνδυνος ανεπιθύμητων αντιδράσεων (Rosemary D. Laird, MD).
Τεκμηριωμένη Συνταγογράφηση (Evidence Based Prescription) – που οδηγεί σε ασφαλή και αποτελεσματική χρήση των Φαρμακευτικών Σκευασμάτων. Εφαρμογή ολοκληρωμένων πρωτοκόλλων και συστηματική επαναξιολόγηση συνταγογράφησης από ιατρό και φαρμακοποιό σε ηλικιωμένους .
Εν κατακλείδι ο περιορισμός του φαινομένου της πολυφαρμακίας μπορεί να επέλθει μέσω της κλινικής και οικονομικής αξιολόγησης των φαρμάκων, του ελέγχου της ιατρικής συνταγογραφικής συμπεριφοράς, και της προαγωγής του θεσμού της Αγωγής Υγείας και Πρόληψης από τους Επαγγελματίες Υγείας, με την οργάνωση και εύρυθμη λειτουργία της Πρωτοβάθμιας Φροντίδας Υγείας (ΠΦΥ) και το θεσμό του προσωπικού ιατρού. Ο ρόλος του ιατρού της ΠΦΥ είναι καθοριστικός, μιας και οφείλει να αναλάβει την ολιστική παρακολούθηση και διαχείριση των ασθενών την ορθολογική συνταγογράφηση και την ενημέρωση για κινδύνους πολυφαρμακίας.
Η εναντίωσή του στην πολυφαρμακία πιστοποιείται και από τη φράση του «πολλές φορές το καλύτερο φάρμακο είναι το κανένα φάρμακο»-Ιπποκράτης .
In English…
As a stakeholder of the European Medicines Agency , I’m an ambassador for Rational Use of Medicines in Health Care. The concept of rational drug use is a fundamental principle in patient care.
Thesis: The problem of Polypharmacy tends to be increasingly recognized as modern plague in our century. When an individual is taking more pharmaceuticals than those that are medically warranted , his/her state of health is put in danger much more seriously by the drug overuse alone rather than by the medical condition for which he/she is being treated itself. The battle, known as polypharmacy, has been estimated to cause the death of 100,000 older adults in USA each year. The unnatural cause of death is the Combined Drug Intoxication (CDI), also known as Multiple Drug Intake (MDI) or lethal polydrug/polypharmacy . It is not supposed to be seen as a drug overdose but as a completely different phenomenon.
I will briefly present you 2 causes for this phenomenon and ways to be prevented.
Polypharmacy refers to the effects of taking multiple medications simultaneously in order to manage coexisting health problems, such as diabetes and hypertension. It is common worldwide among older adults in developed countries ; approximately one third of senior citizens in the United States and Germany and almost two thirds in Canada use 5 or more prescription drugs. However ,patients at highest risk include not only the elderly but also those with multiple comorbid medical conditions. These 2 patient populations often require multiple medications in order for their multiple health-related conditions to be taken care of.
From the patients’ point of view , any remedy will be sought as long as the illness can be cured. Generally, the more drugs a person takes, the greater the risk of adverse reactions and drug interactions resulting in hospitalization, changes in physiology , other adverse health outcomes and even death. Adverse medication outcomes have been estimated as the fourth or fifth leading cause of death in hospitals in USA. These deaths are associated with the prescription and use of too many or even unnecessary medicines at dosages or frequencies higher than therapeutically essential. However, multiple medications are often necessary and may be seen as the best health care treatment for patients . Evidence from numerous studies reveals that many medications prescribed to elderly patients are inappropriate, in that they introduce a significant risk for occurrence of an adverse event especially if there is evidence that alternative medication may be equally or more effective. In primary health care, approximately 1out of 5 prescriptions issued for older adults is inappropriate.
How can this be possible?
Polypharmacy becomes dangerous, when patients are prescribedtoo many medications by multiple healthcare providers working independently from one another. Patients often visit several physicians without revealing the previous prescriptions and continue to take the medications prescribed by all the physicians without the knowledge of multiple-drug interaction and overdose. These drug –to – drug interactions occur when no single healthcare provider is aware of the patient’s complete medication history.
Medication adherence may be defined as “the extent to which a person’s behavior (in this case medication consumption) complies with agreed recommendations made by a health care provider”. It is clear that taking medication is a complex behavior which requires multiple successful steps and efforts to be taken by the patients themselves (i.e., to fill, initiate, continue, and take the prescription as intended).
More specifically, non-compliance on the part of a patient may take one or more of the following forms :
· non-adherence to the standards set by the medication use process,
· non-fulfillment (or primary non-adherence, in cases where a physician prescribes a medication which is never taken by the patient),
· non-persistence (the patient decides to stop taking a medication after having started to take it without being advised by a health professional to do so) and
· non-conformity (the patient takes incorrect doses, skips some doses or takes doses at inappropriate times).
Some of the patients are used to take OTC medications and herbal supplements without a clear knowledge of their efficacy and adverse reactions. When drug side effects occur for some drugs they are often misinterpreted as symptoms of a disease and consequently additional drugs are prescribed by the practitioner.
Solution: As the old adage goes, “an ounce of prevention is worth a pound of cure.”. Measures can and should be taken to limit polypharmacy.
The concurrent use of multiple drugs should be carefully monitored by a qualified professional such as a board certified and licensed medical doctor. A regular review includes assessing appropriateness and on-going need for therapy, adverse effects and interactions, as well as the dosage regime and formulations and the patients’ compliance. In the absence of any pharmacological approach , recourse may be had to lifestyle – related measures whenever possible either in addition to or instead of medications. Always make sure to retain only those medicines for which there is an apparent on-going need to take them and decrease the dosing frequency, when possible.
Draw linkages between each prescribed medication and a specific disease state; each medication prescribed should match the patient’s diagnosis. Any medication that does not match a diagnosis is potentially unnecessary, and efforts to discontinue the medication should be made. Any drug that is unnecessary, inappropriate, or is highly likely to cause side effects that would require additional therapy should not be recommended or dispensed.
What if there was a primary healthcare advocate who would coordinated the overall health care treatment for each patient ?If that was the case , the risk of polypharmacy could be significantly reduced. Effective communication between the healthcare providers taken care of the same patient could play a key role to the elimination of that problem.
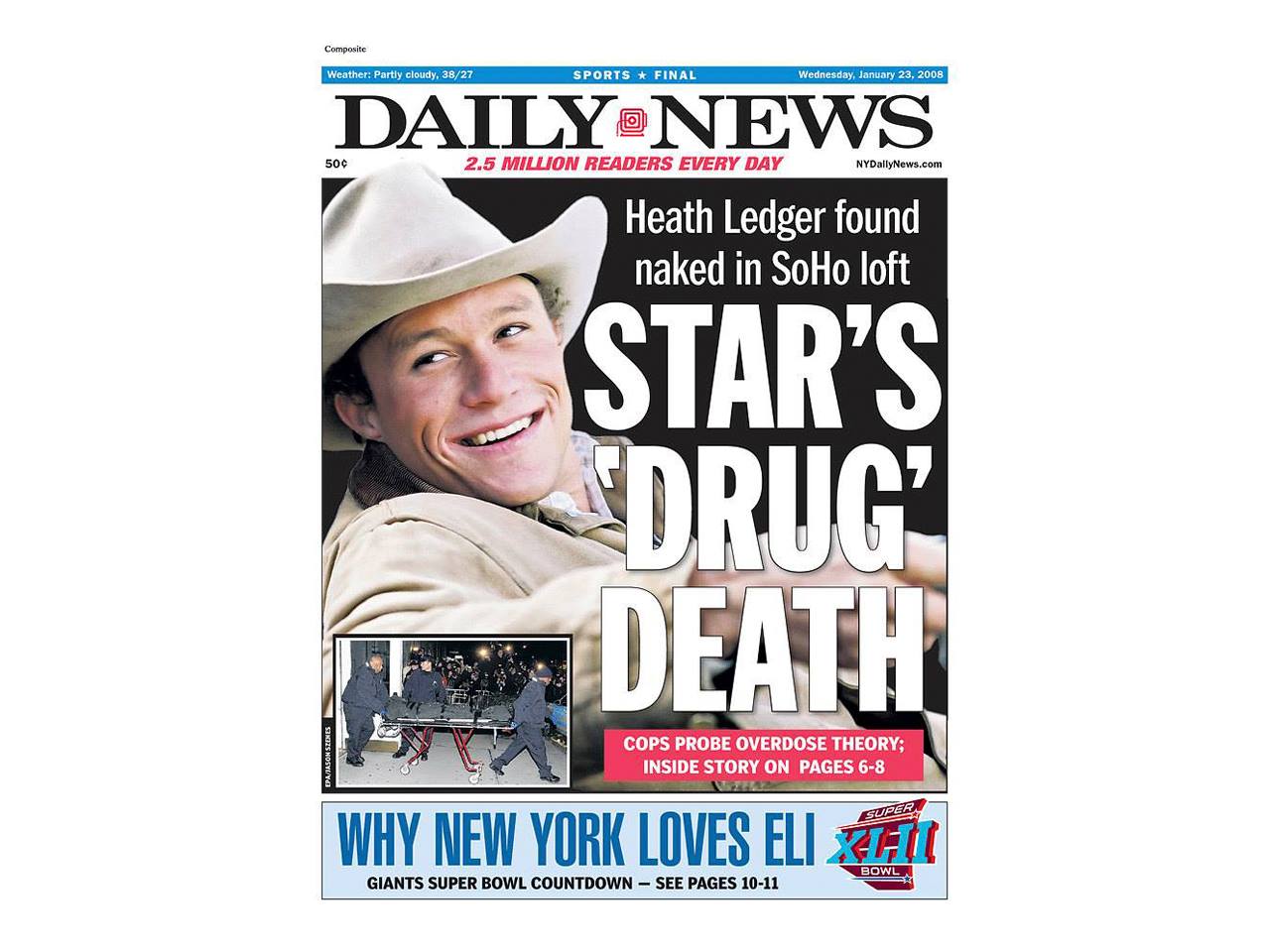
A tragedy when taking several unnecessary medications…
Australian actor Heath Ledger was found dead on January 22, 2008, in his SoHo, New York City, apartment; the toxicology report described the cause of death was “acute intoxication” resulting from “the combined effects of oxycodone, hydrocodone, diazepam, temazepam, alprazolam, and doxylamine” and concluded “that the way in which he died was a result of the abuse of prescription medications or combine drug intoxication (CDI).
Asking the right questions is crucial to minimize the risk of harm to the patient !
One of the most famous Hippocrates quotes goes along the following lines : “ The greatest medicine of all is to teach people how not to need it”.